Olympics inspired you to start running?
Pounding the pavement during lockdown?
Let’s talk Tendinopathies!
 Since the start of the pandemic everybody seems to have picked up a new hobby or two! While, many of us have found a new passion, a silver lining in an otherwise uneventful period, many have walked through our doors with injuries directly related to their new found past time. So, before you try and become the next Cathy Freeman or Steve Mongehetti lets discuss one of the most common running injuries, tendinopathy!
Since the start of the pandemic everybody seems to have picked up a new hobby or two! While, many of us have found a new passion, a silver lining in an otherwise uneventful period, many have walked through our doors with injuries directly related to their new found past time. So, before you try and become the next Cathy Freeman or Steve Mongehetti lets discuss one of the most common running injuries, tendinopathy!
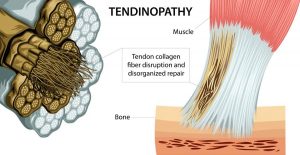
Tendinopathy is a common word thrown around by many budding athletes to describe an injury. Tendinopathies also go by their other aliases: Tendonitis, tenosynovitis and tendinosis. In simple terms, they are terms used to describe a tendon injury pathologies, but the now the universally accepted term of Tendinopathy is most commonly used. In this article we will explore the pathology behind a Tendinopathy…
What is a Tendon?
A tendon is a fibrous band of connective tissue that connects a muscle to the bone. It is created via interwoven collagen fibres, creating a strong anchor point for the muscle to attach. Tendons are often confused with ligaments, which run between two bones
Where and when do Tendon injuries occur?
Tendon’s are found all over the human body but the most common injury sites for runners occur at the achilles and patella tendons.
Most tendon injuries at 3 different locations within the tendon itself:
- tendon insertion (i.e. where the tendon attaches to the bone)
- mid-tendon (non-insertional tendinopathy)
- musculotendinous junction (where the tendon attaches to the muscle)
Of these locations, the greater majority occur at the tendon insertion and are the direct result of repeated overloading. These are known as Insertional Tendinopathies.
 What are the symptoms of Tendinopathy?
What are the symptoms of Tendinopathy?
Tendinopathy typically causes pain, stiffness and loss of strength in the affected area/s. Other common issues include:
- Worsening pain with use
- Increased pain or stiffness during the night or first thing in the morning
- Tenderness, redness, warmth and swelling
- Often occur in the presence of a bursitis injury
The Four phases of a Tendinopathy
If your tendon is failing to adapt to the daily loads being placed on it, it will typically pass through four stages of degeneration:
1. Reactive Tendinopathy:
Normal tissue adaptation phase during training periods, with an excellent prognosis and normal recovery period
2. Tendon Dysrepair
Rate of tendon degeneration is faster than that of tissue repair. This is the critical phase to address your current training load, as this will ensure that the loading does not continue to overwhelm the healing process. This is the most common phase seen by Physiotherapists, with a generally good prognosis if managed appropriately!
3. Degenerative Tendinopathy
Chronic injury phase in which tendon cell death is occurring and rapid deterioration in function is experienced. The prognosis for interventions at this stage is poor.
4. Tendon tear/Rupture
The final and most catastrophic phase, in which significant tissue breakdown has occurred, with a near/total loss of function in the tendon. The prognosis at this stage is very poor and usually surgical interventions are the only option
Treatment?
 Based on the four phases noted above, the treatment for a Tendinopathy will widely vary and will also be affected by other factors such as age, gender, sporting background, previous injury etc. Tendinopathies can be treated effectively and efficiently if the phase of the Tendinopathy is identified, and treatment begins during the earlier stages. Returning to sport and physical activity should be guided by your treating physiotherapist to ensure that appropriate rehabilitation has taken place and your tendon is in a position to tolerate the loading you will place on it!
Based on the four phases noted above, the treatment for a Tendinopathy will widely vary and will also be affected by other factors such as age, gender, sporting background, previous injury etc. Tendinopathies can be treated effectively and efficiently if the phase of the Tendinopathy is identified, and treatment begins during the earlier stages. Returning to sport and physical activity should be guided by your treating physiotherapist to ensure that appropriate rehabilitation has taken place and your tendon is in a position to tolerate the loading you will place on it!
Summary
In summary, tendon’s like to be loaded for growth, however, the right loads are critical! Just as Cathy and Steve would have started, its best to begin slowly and load progressively without ‘shocking’ the tendons by placing them under too much load too quickly! Consider the latter a one-way ticket into the MGS clinic! See you on the pavement 🙂
